About Myelofibrosis
What is myelofibrosis?
- Myelofibrosis is a blood cancer characterized by the buildup of excessive scar tissue in the bone marrow, which interferes with the production of healthy blood cells.1
- In the U.S., approximately 25,000 people are affected by myelofibrosis.2
- Myelofibrosis can lead to severe low blood counts, including anemia and thrombocytopenia (low platelet count), as well as constitutional symptoms, such as weight loss, fatigue, and splenomegaly (enlarged spleen).1,3
- Some currently approved treatments for myelofibrosis exacerbate anemia, leading to a more than 30% discontinuation rate.4
- There remains a significant medical need for myelofibrosis patients with anemia, which is associated with a negative impact on overall survival and quality of life.4
What are the signs and symptoms of myelofibrosis?
- In early stages, approximately 1/3 of people impacted by myelofibrosis do not have symptoms of the disease.5
- However, as the disease progresses, some of the signs and symptoms that people may experience include:4,5
- Anemia
- Bone or joint pain
- Easy bleeding or bruising, because of a low platelet count (thrombocytopenia)
- Enlarged liver
- Excessive night sweats
- Fever
- Frequent infections, due to a low white blood cell count (neutropenia)
- Itching
- Pale skin
- Splenomegaly, or enlarged spleen, resulting in pain or a feeling of fullness below the ribs on the left side
- Tiredness
- Weakness, or shortness of breath that is usually attributed to low red blood cell count
- Weight loss or malnutrition
Who is at increased risk for myelofibrosis?1,6,7
- While everyone can be impacted by myelofibrosis, certain risk factors can increase the likelihood that a person will develop myelofibrosis, including:
- Age
- Myelofibrosis is most commonly diagnosed in people over the age of 64.
- JAK2 Mutation
- Approximately 50% to 60% of people with myelofibrosis have a mutation of the JAK2 gene, which signals blood cells to grow and divide even when the body doesn’t want more.
- Another blood disorder
- Some people may develop myelofibrosis as a result of complications due to essential thrombocytopenia or polycythemia vera.
- Exposure to certain chemicals.
- Exposure to industrial chemicals, such as toluene and benzene, have been linked to myelofibrosis.
- Exposure to radiation
- Those who are exposed to very high levels of radiation are at an increased risk of developing myelofibrosis.
- Those who are exposed to very high levels of radiation are at an increased risk of developing myelofibrosis.
- Age
How is myelofibrosis diagnosed?6
- Diagnosis is based on the 2017 WHO Criteria and requires a combination of clinical, laboratory, cytogenetic, and molecular tests, which include:
- Physical exam
- A physical exam may include a check of your vital signs, such as pulse and blood pressure, along with checks of the lymph nodes, spleen and abdomen.
- Blood tests to check for low blood cell and platelet counts
- One test looks at your complete blood count, which may show abnormally low levels of red blood cells, indicating potential anemia. White blood cell and platelet counts are also looked at and may be higher or lower than normal in some people.
- X-rays and MRIs
- Imaging tests such as X-rays and MRIs can help your doctor determine more information about your myelofibrosis.
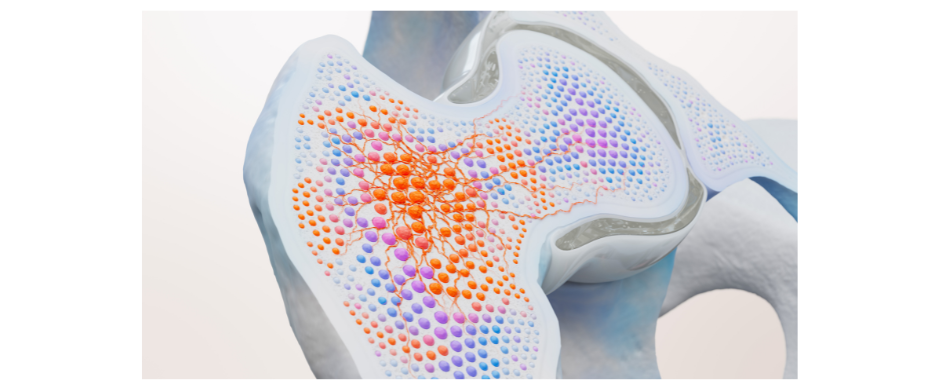
- Bone marrow biopsy
- A sample of bone tissue and marrow from your hipbone is extracted using a needle. Another type of needle may also be used during the procedure, to withdraw a sample of the liquid portion of your bone marrow. The samples are studied in a laboratory to determine the numbers and types of cells found.
- Testing cancer cells for abnormal gene mutations, such as JAK2, CALR and MPL
- These tests can help inform your prognosis and potential treatment options.
- These tests can help inform your prognosis and potential treatment options.
- Physical exam
How is myelofibrosis treated?6
- The goal of treatment for people with myelofibrosis is to reduce symptom burden and minimize the risk of developing acute leukemia, a cancer that progresses rapidly. Based on the symptoms you’re experiencing, your doctor might recommend treatment for anemia (i.e., blood transfusions, medications), enlarged spleen (i.e., chemotherapy, removal of the spleen, radiation therapy) and/or thrombocytopenia.
- In addition to these treatments, some patients are eligible for a bone marrow transplant, also known as an allogenic stem cell transplant. This procedure involves replacing disease bone marrow with healthy blood stem cells from a donor. This treatment has the potential to cure myelofibrosis.
If you or someone you know has myelofibrosis, getting to the right care is key. Myelofibrosis symptoms can present and progress differently for everyone. Talk to your healthcare professional about any signs and symptoms you may be experiencing. Your healthcare professional can help refer you for the right testing and help you navigate potential treatment options that may be right for you.
Mapping Myelofibrosis
Mapping Myelofibrosis was created to increase awareness of this blood cancer, which can be difficult to diagnose. Whether you, or someone you care for, has been living with this disease for years, or is experiencing symptoms without a diagnosis, Mapping Myelofibrosis connects the community with educational tools, resources, and stories to help navigate all aspects of the disease.
• For those who have not been diagnosed, early detection of the disease may be beneficial.
• For those who have been diagnosed, understanding your symptoms is key to making informed decisions with your healthcare providers.
This initiative is being developed with input from MPN Research Foundation (MPNRF)
and MPN Advocacy & Education International (MPN A&E).
MPNRF is an independent body bringing together the voices of the patient and their caregivers living with a MPN and the researchers and clinicians seeking answers for MPN patients. MPNRF supports multiple efforts to increase awareness of MPNs and advancements of all validated, promising, and impactful approaches to better outcomes for patients.
MPN A&E International provides educational programs, materials, and resources for patients, caregivers, physicians, and entire healthcare teams to improve their understanding of myelofibrosis, polycythemia vera, and essential thrombocythemia. They are dedicated to making a difference in the lives of those affected by MPNs and strive to grow awareness and advocate on behalf of the entire MPN community.
References
1 MPN Research Foundation. Primary Myelofibrosis (PMF). Accessed March 2023. http://www.mpnresearchfoundation.org/primary-myelofibrosis-pmf/
2 Data on file. Sierra Oncology. 2021.
3 NIH National Library of Medicine. Primary Myelofibrosis. Accessed March 2023. https://medlineplus.gov/genetics/condition/primary-myelofibrosis/
4 Kuykendall AT, Shah S, Talati C, et al. Between a rux and a hard place: evaluating salvage treatment and outcomes in myelofibrosis after ruxolitinib discontinuation. Ann Hematol. 2018;97(3):435-441.
5 Cleveland Clinic. Myelofibrosis. Accessed March 2023. https://my.clevelandclinic.org/health/diseases/15672-myelofibrosis
6 Mayo Clinic. Myelofibrosis. Accessed March 2023. https://www.mayoclinic.org/diseases-conditions/myelofibrosis/diagnosis-treatment/drc-20355062#:~:text=Imaging%20tests%2C%20such%20as%20X,confirm%20a%20diagnosis%20of%20myelofibrosis
7 O’Sullivan JM, Harrison CN. Myelofibrosis: clinicopathologic features, prognosis, and management. Clin Adv Hematol Oncol. 2018;16(2):121-131.