While the concept of synthetic lethality was first described in 1922, it was not until 2005 when the discovery of the first synthetic lethal interaction was able to be translated into the clinic for patients with cancer [1],[2],[3],[4]. This paved the way for a new wave of genetically selective cancer medicines that largely leave a patient’s healthy cells unharmed.[4]
A synthetic lethality-based treatment strategy has two major advantages: firstly, it can be utilized against the majority of cancer mutations and secondly it allows us to identify patients who are most likely to respond to treatment.
Synthetic lethality is a new strategy for developing anticancer therapies where the functional loss of individual genes are tolerated in isolation but not in combination. It happens when a combination of deficiencies in the expression of multiple genes lead to cell death.
Synthetic lethality can be applied in drug discovery to develop medicines that target specific genetic mutations expressed only in cancer cells, and not present in normal cells.[4] Genetics play a heavy role in progression of the disease; therefore, patients who would benefit the most from a synthetic lethal therapy can be preselected based on their genetic profile, increasing the likelihood of response and reducing toxicity.[4],[5]
What is synthetic lethality?
Synthetic lethality is a new strategy for anticancer therapies where two genetic abnormalities that act independently and are not lethal become lethal when combined in the same cell. It happens when a combination of deficiencies in the expression of multiple genes lead to cell death.
Exploiting pro-cancer mutations to develop anticancer medicines
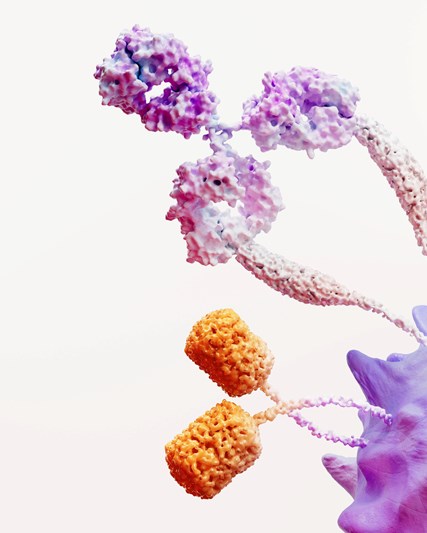
In cancer, the concept of synthetic lethality applies to pairs of genes.[4] Tumor suppressor genes are genes that control cell growth. The loss of ‘tumor suppressor’ gene function is a central mechanism to turn normal cells into cancer cells, often by causing or allowing a large number of mutations in the genome.[4] Tumor suppressor gene loss is not something that we can target with medications, as the genes themselves are often already mutated or deleted in cancer and therefore anticancer medicines cannot directly interact with them.[4]
As tumor suppressor genes cannot be directly targeted, we can leverage synthetic lethality by targeting the gene partner. We target the gene partner with a synthetic lethal drug to inhibit its function;[4] this leads to death of cancer cells whereas normal cells that retain function of the related tumor suppressor gene are spared this effect.[4] Identification of druggable synthetic lethal partners is currently the only way of targeting the functional loss of tumor suppressor genes in cancer.[4]
The first synthetic lethal interaction found in cancer was between poly (ADP-ribose) polymerase (PARP) and tumor suppressor genes BRCA 1 and 2. Gene products of PARP and BRCA1/BRCA2 normally function to repair DNA damage.[4] During the development of certain cancers, genes such as BRCA1/BRCA2 are mutated and non-functional, which limits the repair of DNA in these cancer cells to only utilizing PARP. If we use a PARP inhibitor, we can make PARP repair non-functional and the cancer cells sensitive to cell death; this is a practical example of synthetic lethality, which largely spares a patient’s healthy cells.[4]
Exploiting the synthetic lethal concept in the DNA damage repair pathway is currently of high interest to me. It now appears that a clinically significant fraction of cancers do have DNA repair defects.
Research underpinned by the search for genetic interactions
In order to discover new synthetic lethal gene pairs, we need to use new technologies that change our approach and enhance our ability to understand the research in the space. When you consider the exponential number of potential synthetic lethal gene pairs in the human genome, this requires an approach that collects vast amounts of data.[4]
For many years, data was obtained through genetic screening for loss-of-function mutations in yeast or by use of genetic tools in human/mammalian cells, however these technologies were limited by the reliance on conserved genes (those that have been unchanged throughout evolution and are present across species), or inaccuracies when experiments were scaled up.[4],[6],[7],[8] Today CRISPR (clustered regularly interspaced short palindromic repeats)-based tools and libraries offer a path forward, where ‘hits’ (i.e. potential drug targets) can be generated, and the patient population expected to benefit from inhibiting each target is already known.[4]
Over the next five to ten years, I hope research leads us to identify novel synthetic lethal partners beyond PARP inhibition and BRCA mutation to help expand the patient population that can benefit from this science.
Building synthetic lethality from concept into reality at GSK
CRISPR-based tools have revolutionized the discovery of several synthetically lethal combinations that are currently in clinical trials. This progress demonstrates the potential of CRISPR technology to dramatically alter cancer target discovery and create a wave of new therapeutics over the next decade.[4],[9]
At GSK, our industry-leading synthetic lethality research unit is working to advance our preclinical program capacity while further understanding the underlying mechanisms of synthetic lethality drug resistance. Our larger vision in R&D is to identify novel targets in drug-resistant patient populations, underpinning our goal to deliver potentially transformational medicines in oncology.
In June of 2020, GSK and IDEAYA Biosciences formed a strategic partnership to advance three novel synthetic lethality assets, including as monotherapy and as combinations between GSK and IDEAYA programs. This partnership enables compelling potential combinations and the opportunity to build an industry leading pipeline that targets molecularly defined populations in several major solid tumors. The collaboration has the potential to bring the next generation of innovative precision medicine therapies to patients utilizing the approach of synthetic lethality, and could have meaningful impact for the clinical care of patients with lung, prostate, breast, colorectal and ovarian cancers.
References
[1] Bridges, C. The origin of variations in sexual and sex-limited characters. Am. Nat. 1922;56(642):51-63.
[2] Farmer H, McCabe N, Lord CJ, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434(7035):917-21.
[3] Lord CJ, Ashworth A. PARP inhibitors: Synthetic lethality in the clinic. Science. 2017;355(6330):1152-8.
[4] Huang A, Garraway LA, Ashworth A, et al. Synthetic lethality as an engine for cancer drug target discovery. Nat. Rev. Drug Discov. 2019;11:1-6.
[5] > Behan FM, Iorio F, Picco G, et al. Prioritization of cancer therapeutic targets using CRISPR–Cas9 screens. Nature. 2019;568(7753):511-6.
[6] Kaelin WG. Choosing anticancer drug targets in the postgenomic era. J Clin Invest. 1999;104(11):1503-6.
[7] Kaelin WG. The concept of synthetic lethality in the context of anticancer therapy. Nat. Rev. Cancer. 2005;5(9):689-98.
[8] Hartwell LH, Szankasi P, Roberts CJ, et al. Integrating genetic approaches into the discovery of anticancer drugs. Science. 1997;278(5340):1064-8.
[9] Jariyal H, Weinberg F, Achreja A, et al. Synthetic lethality: a step forward for personalized medicine in cancer. Drug Discov. Today. 2020;25(2):305-20.