GSK has successfully innovated treatments that have transformed the management of some of the most prevalent and serious lung conditions, including chronic obstructive pulmonary disease (COPD), asthma and the respiratory syncytial virus (RSV).
GSK’s most recent R&D work in the respiratory space has reinforced the criticality of controlling inflammation in patients living with COPD and asthma. Like many chronic illnesses, these respiratory conditions are still often misunderstood. While every patient experiences their disease differently, one dangerous commonality is the risk of a sudden worsening of symptoms known as exacerbations or flare-ups.
Flare-ups occur when existing respiratory symptoms suddenly become more severe, such as a person’s inability to catch their breath. When we see increases in the frequency and severity of flare-ups, this can signal a more serious pathology. Worsening flare-ups can last for days or weeks and result in hospitalization. One in four patients hospitalized for COPD exacerbation return to the hospital for an acute exacerbation within 30 days, and almost 90% of patients are readmitted to the hospital within a year.1
Preventing flare-ups is key to disease management
Asthma affects individuals differently, leading to a wide range of experiences. While some people with asthma may experience infrequent flare-ups, others face the significant challenge of multiple daily attacks. These attacks, characterized by symptoms like wheezing, shortness of breath, chest tightness, and coughing, can range in severity. For some, disrupting daily activities, work, school, and overall quality of life. Understanding the potential for both mild and severe attacks is key for effective asthma management and preparedness.
For people living with COPD, flare-ups can be triggered by anything that causes breathing issues. They are surprisingly common and even people taking daily maintenance inhalers are susceptible, with up to 50% of people living with COPD continuing to experience flare-ups despite maintenance inhalers.2 Every flare-up increases the chance of having another flare-up, which leads to approximately 900,000 emergency room visits per year.3 Some patients also have a specific type of inflammation that could lead to even more frequent flare-ups, and aggravate existing comorbidities, such as heart disease or metabolic disorders, compounding the overall health burden. This is why preventing flare-ups, including those that require hospitalization, is critical to successful disease management.
Beyond the immediate medical ramifications, flare-ups make ordinary daily life even more challenging.

“The stress and uncertainty can make it harder to manage work, school, family life, and travel,” said Tonya Winders, President & CEO, Global Allergy & Airways Patient Platform. Knowing that a single flare-up can cause additional flare-ups can be a source of anxiety and depression, and the unpredictability of a flare-up sending you to the hospital significantly impacts planning and even enjoying everyday activities.”
The stress of living with COPD was expressed in a recent COPD focus group where patients reflected on the psychological realities of living with the condition. “I don't want to burden my family with my disease,” one patient confided. “They know I have it. They know that I don't walk long distances if we go to a park. I don't want to be a burden.” Another patient added, “I get too emotional talking about my disease, so I prefer to stay home and not have to explain myself.”
Inflammation is a stealth culprit in flare-ups
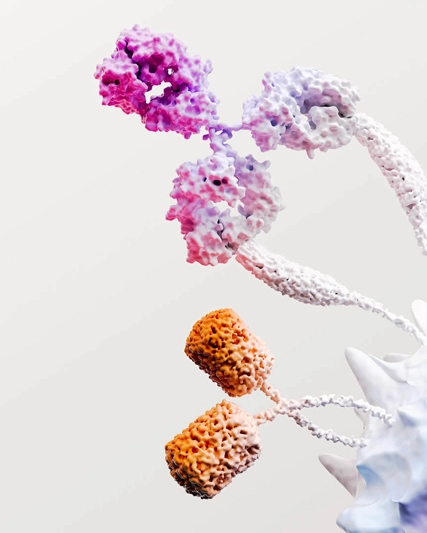
A growing body of scientific research shows that both COPD and asthma symptoms, particularly flare-ups, may be caused by type 2 inflammation. Approximately one-third of people living with COPD4 and approximately 40% of people living with severe asthma have a blood eosinophil count (BEC) that indicates type 2 inflammation.5 Including a blood eosinophil test in routine screenings, combined with your doctor’s evaluation and diagnostic tools, can provide valuable information to inform a diagnosis and subsequently determine an appropriate treatment plan to reduce flare-ups.

“We continue to advance our understanding of the role eosinophils play in respiratory inflammation – work that could have profound implications on our ability to help COPD patients prevent exacerbations and reduce hospitalizations and emergency room visits,” said Emmeline Burrows, US Medical Affairs Lead, Respiratory, GSK. “Patients who are following their prescribed maintenance inhalers but still suffering at least one flare-up a year should consider asking their doctor for simple blood testing to check their blood eosinophil counts, which, along with other medical assessments, can help determine the appropriate management of their condition. While we know many of the key drivers of COPD, having a better understanding of underlying Type 2 inflammation is crucial for developing more effective treatments to help people with COPD.”
References
Ruan H, et al. Readmission rate for acute exacerbation of chronic obstructive pulmonary disease: A systematic review and meta-analysis. Respir. Med. 2023, 206, 107090. https://www.resmedjournal.com/article/S0954-6111(22)00355-9/fulltext.
Rabe KF, et al. Triple inhaled therapy at two glucocorticoid doses in moderate to very severe COPD. N Engl J Med; 2020;383:35-48. https://www.nejm.org/doi/pdf/10.1056/NEJMoa1916046.
American Lung Association | COPD Trends Brief | Available at www.lung.org.
Tashkin DP, Wechsler ME. Role of eosinophils in airway inflammation of chronic obstructive pulmonary disease. Int J COPD. 2018;13:335-349. doi:10.2147/COPD.S152291.
Laurits F., et al. The prevalence of subtypes of type 2 inflammation in an unselected population of patients with severe asthma. The Journal of Allergy and Clinical Immunology: In Practice; 2021;9 1267-1275. https://doi.org/10.1016/j.jaip.2020.09.051.