A new survey suggests that more open and honest conversations about the impact of chronic obstructive pulmonary disease (COPD) between patients, their caregivers and their doctors are needed.
These survey findings reveal an opportunity for people living with COPD and their caregivers to play an active role in the management of their disease and shed light on how to change the conversation to improve COPD care.
The survey, developed and conducted by GSK in collaboration with the CHEST Foundation and the COPD Foundation, gathered insights from 351 people with COPD, 151 caregivers and 501 physicians who treat COPD in the U.S.
COPD and COVID-19 Pandemic
The COVID-19 pandemic has had a significant impact on people with COPD and their care teams, both positively and negatively.
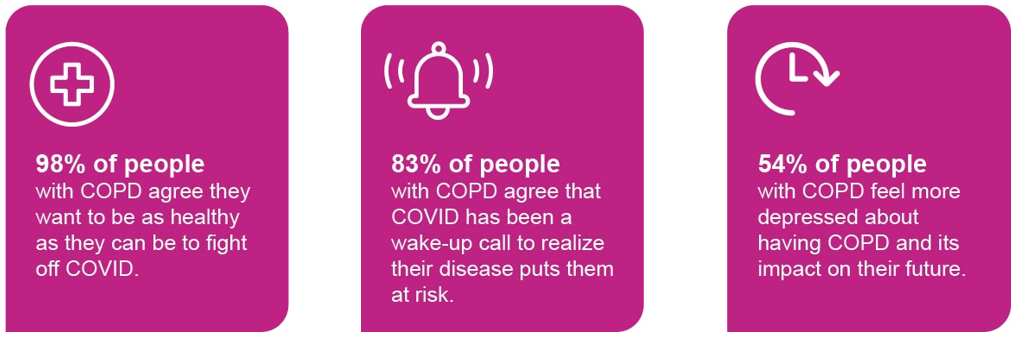
Despite an increase in motivation to better manage their disease, the survey showed patients are still settling for symptoms that impact their daily routines and holding them back from doing what they love.
Settling for a ‘New Normal’
People with COPD are settling for a life of significant, disruptive symptoms, such as avoiding going outside the home, canceling plans with family and friends or having trouble sleeping.
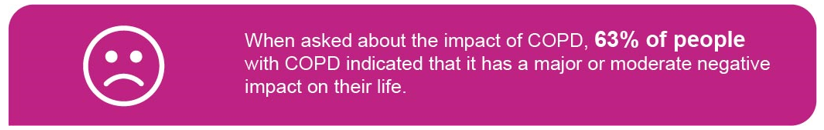
Despite the negative impact of COPD, caregivers report people with COPD aren’t speaking up enough about their disease. In fact, 56% of caregivers reported hearing their loved one downplay symptoms during medical appointments at least half of the time.
COPD is a chronic and progressive inflammatory lung disease that affects roughly 27 million people in the U.S. It obstructs a person’s airways, making it difficult to breathe. While there is no cure for COPD, it can be well-managed with careful disease management and more open and honest conversations about the impact of the disease.
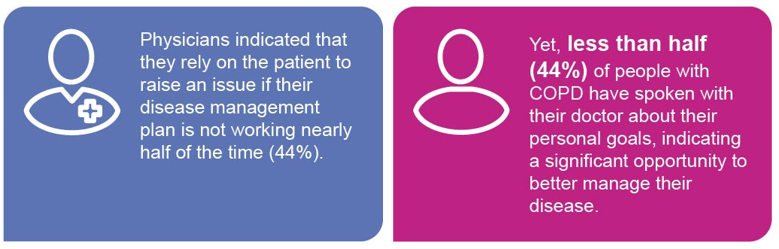
Unfortunately, many people with COPD (46 percent) have resigned to the belief that disruptive symptoms are a normal part of their disease and that there is nothing they or their physician can do. Further, when people with COPD don’t feel their disease management plan is working, less than a third (30%) of those we surveyed admitted they had asked their healthcare team for it to be reviewed and reevaluated.
That doesn’t have to be the case.
People with COPD do not have to live with negative and disruptive symptoms. Open and honest communication is the first step to addressing that.
Caregiver Involvement
Caregivers play a crucial role in helping facilitate productive discussions during doctor’s appointments helping to ensure their loved ones receive optimal care. Their involvement helps paint a clear picture of the patient’s routine and symptoms at home for the physician.
Caregivers also support early identification of signs of disease progression and ensuring people with COPD adhere to their medication.
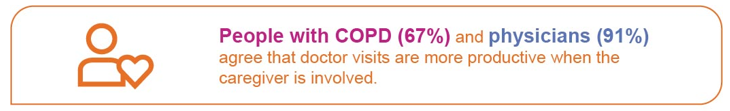
Despite current barriers to optimal COPD care, there are opportunities to improve disease management – most notably, the absolute need for improved patient-physician communication, with the help of a caregiver. A great first step for people living with COPD and their caregivers is to bring a list of questions or notes about symptoms to appointments. For physicians, start with revisiting discussions with patients who continue to struggle with managing their COPD.
Many people with COPD feel guilty about having the disease and tend to believe there is nothing their physician can do to improve it. They must know that’s not the case – better days are possible through consistent and comprehensive disease management.
To learn more about COPD symptoms and ways to improve gaps in COPD communication, visit copd.com




