Myelofibrosis (my-ah-lo-fye-BRO-sis) (MF) is a complex blood cancer. It is part of a bigger group of blood cancers called myeloproliferative neoplasms, or MPNs. Each person experiences myelofibrosis differently – and navigating the symptoms can be daunting. Those affected by myelofibrosis may find themselves in uncharted territory, feeling isolated, lost and unsure where to turn to for education, resources and support.
..............................................................................................................................................................................................................................................................................................
Mapping Myelofibrosis was created to increase awareness of this blood cancer, which can be difficult to diagnose. Whether you, or someone you care for, has been living with this disease for years, or is experiencing symptoms without a diagnosis, Mapping Myelofibrosis connects the community with educational tools, resources, and stories to help navigate all aspects of the disease.
- For those who have not been diagnosed, early detection of the disease may be beneficial.
- For those who have been diagnosed, understanding your symptoms is key to making informed decisions with your healthcare providers.
This initiative is being developed with input from MPN Research Foundation (MPNRF)* and MPN Advocacy & Education International (MPN A&E)
MPNRF is an independent body bringing together the voices of the patients and their caregivers living with an MPN and the researchers and clinicians seeking answers for MPN patients. MPNRF supports multiple efforts to increase awareness of MPNs and advancements of all validated, promising, and impactful approaches to better outcomes for patients.
MPN A&E International provides educational programs, materials, and resources for patients, caregivers, physicians, and entire healthcare teams to improve their understanding of myelofibrosis, polycythemia vera, and essential thrombocythemia. They are dedicated to making a difference in the lives of those affected by MPNs and strive to grow awareness and advocate on behalf of the entire MPN community.
Mapping Myelofibrosis Podcast
The Mapping Myelofibrosis podcast is sponsored by GSK. Through conversations with a variety of guests across the myelofibrosis community, our aim is to shed light on the significant medical needs patients face and deliver helpful tips for patients, caregivers, and advocates alike.
Our first episode features Cheryl Petruk, Executive Director and Founder of the Canadian MPN Research Foundation and also Executive Director of the Canadian MPN Network. Watch below as Cheryl shares her husband’s journey with myelofibrosis as well as her own perspective as a caregiver. Stay tuned for more conversations as part of the ongoing Mapping Myelofibrosis program.
Transcript
TEXT ON SCREEN:
Mapping Myelofibrosis Logo
GSK presents
Mapping Myelofibrosis
A Caregiver’s Journey
Jasmine Sahni, Host
JASMINE SAHNI:
“Hi everyone. My name's Jasmine Sahni. I'm a global scientific director with GSK.”
TEXT ON SCREEN:
Cheryl Petruk, Myelofibrosis Caregiver and Advocate
JASMINE SAHNI:
“Today, joining me, is Cheryl Petruk. She’s the founder of the Canadian MPN Research Foundation. We’ll be talking a little bit about myelofibrosis overall, as well as the impact on caregivers and what that’s like for the families of loved ones suffering with myelofibrosis.”
“So, Cheryl, thank you again for joining me today. Can you tell us a little bit more about your husband's journey and what it was like for you from the caregiver aspect?”
CHERYL PETRUK:
“Absolutely. So in 1991, my husband was diagnosed with essential thrombocythemia. We were actually trying to conceive to have children, and he had a chest pain. So I urged him to go to the doctor, and he was then diagnosed with having too many platelets in his blood. Essential thrombocythemia. So from then he sought, a second opinion from a hematologist, and the hematologist literally told us, we don't know much about this, even though it had been around for many years.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“It was a blood disorder back then in 1991. And he said, well, you can either live your life, watch and wait and we'll monitor your blood or we'll put you on a drug to suppress the bone marrow. So my husband, Eugene, decided to live his life. We wanted to still have more children. But we did everything that we needed to, just in case.”
JASMINE SAHNI:
“Mm-hmm.”
CHERYL PETRUK:
“And so, we lived our life and, you know, he, we thought he was pretty asymptomatic. He had his blood checked every three months for other medication that he took. And then in 2010 the doctor phoned us, the GP phoned us at home on a Sunday afternoon and said, I think you need to come in and see me.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“And within three days, we were in to see an oncologist at the Cross Cancer Center in Edmonton. And within the hour he said to us, he said, I, I know what you have.”
TEXT ON SCREEN:
About Myelofibrosis & MPNs
JASMINE SAHNI:
“For folks joining us who aren't too familiar, so just to level set, so myelofibrosis, it's, it's a rare blood cancer, a rare cancer of the bone marrow.”
CHERYL PETRUK:
“Yes.”
JASMINE SAHNI:
“It's in a family of diseases called the MPNs. So your husband was initially diagnosed with one form of MPN, and at that point it wasn't even clear that it was actually a cancer.”
CHERYL PETRUK:
“We were never told it was a blood cancer. We were told back in 1991 that it was a blood disorder.”
JASMINE SAHNI:
“Mm-hmm.”
CHERYL PETRUK:
“And that you could live a long, long life with it. And that they saw it mostly in older people.”
JASMINE SAHNI:
“Mm-hmm. Retrospectively, like knowing what you know now, what were some of the signs that were signs of progression that may have seemed ordinary at the time? Or-.”
CHERYL PETRUK:
“You know, fatigue being one of them. That's probably the biggest one. You know the early satiety. You know, we were both trying to lose weight and his was coming off a lot quicker. And I would look at him and go, "Why are ... you know, we're eating the same things. You're losing more weight than I am and-.”
JASMINE SAHNI:
“Frustrating.”
CHERYL PETRUK:
“Frustrating. Absolutely. And you know, so the fatigue and the weight loss, the early satiety. He literally, you know, as he transformed from ET to myelofibrosis you know, the fatigue. He had a desk job, he, you know, he worked in an office. So it wasn't like he was extremely active, but he would come home and you know, be really fatigued, not being able to do a whole lot.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“The early satiety, you know, he couldn't eat a lot because his spleen was growing.”
CHERYL PETRUK:
“You know, he looked and, you know, most people when you lose weight, you lose, you know, that belly fat and, and whatnot. But his wasn't, his spleen was growing. It was literally the size of a, of an NFL football. He looked nine months pregnant, you know, in.”
JASMINE SAHNI:
“I see.”
CHERYL PETRUK:
“In the very end. And we just couldn't put our, you know, like, is it too much stress? Is it this, is it that. You know, he just felt like he said, but I feel like I have a knot. You know, something pushing on my stomach. So, yeah, absolutely. There were signs, but we didn't know that those were signs of progression at all.”
JASMINE SAHNI:
“I see. And over that time from when he was diagnosed with myelofibrosis, I mean, I in the beginning, I assume those changes in signs were slowly evolving you know, compared to, you know, 10 years later.”
CHERYL PETRUK:
“Absolutely.”
JASMINE SAHNI:
“Okay.”
CHERYL PETRUK:
“Absolutely. So, yeah. You know one of the other signs that he had was he had a lot of bruising all over his body. And so very bad, eggplant purple bruises. And, you know, his doctor said, oh, you know, your muscles, maybe they're just tearing or maybe there's something happening.”
JASMINE SAHNI:
“Oh, that was happening before the actual myelofibrosis.”
CHERYL PETRUK:
“Absolutely. Or, you know, in the transition when he was progressing, before it was actually diagnosed that he had progressed.”
JASMINE SAHNI:
“I see.”
CHERYL PETRUK:
“To myelofibrosis.”
JASMINE SAHNI:
“So then how many, how long after did you, or did he feel the enlarged spleen and some of the other signs and symptoms?”
CHERYL PETRUK:
“Oh, continually. So from, in 2010 when he was diagnosed with myelofibrosis.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“Yeah. The spleen got larger. You know every time he went to the clinic visit, the doctor always measured his spleen. And it, you know, in the end it was like 29 centimeters. 2010 was kind of that, that turning point. And he was good till about 2014.”
JASMINE SAHNI:
“Okay.”
CHERYL PETRUK:
“Where the hematologist said, you know, let's just watch and wait and monitor, um, monitor this. Because at that point, he wasn't on any medication, in any way. And so.”
JASMINE SAHNI:
“For the anemia you mean?”
CHERYL PETRUK:
“For anything. I always looked at him and when we left the hematologist and said, you know what, I consider this a win. When he said, see you in six months, or see you in, you know, whatever timeframe.”
TEXT ON SCREEN:
Patient & Caregiver Perspectives
JASMINE SAHNI:
“For new patients that you meet, folks who are just getting diagnosed. From a caregiver perspective, what would be your advice to folks who are seeing their loved ones or, you know, family members going through this, you know, from your, from your journey with it, what's something that you would, you know, like to impart with them?”
CHERYL PETRUK:
“Absolutely. You know, one of the things I felt it was my job was, you know, not only to be his caregiver, but to be his care partner. And so, you know, attend to his needs, attend to the needs of the, the physical disability or the mental anguish or the anxiety, you know, reassuring him that he's gonna be okay and that we're gonna live a long life. But from the care partner perspective, I felt it was my job to research. I felt it was my job to find out as much as I could about the disease.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“So that we could navigate the journey. And so that was one of the things that I would, or one of the things that I learned that I would give advice to anyone else is, is, you know there's things that we can do as caregivers. And we can make them feel better, or we can make them feel more comfortable in a situation. But from a care partner perspective, it's your job to do all that backend stuff.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“Because the patient is really trying to live their life.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“And they're trying to focus on being well and being healthy and being in that mental spot of living the best that they can. So as a care partner, I felt it was my opportunity or my duty to get all the research, get, you know, find out about the different clinical trials, find out about the different treatments and communicate with the doctor.”
JASMINE SAHNI:
“Yeah. And what were those resources like? Where did you lean to because myelofibrosis 10 years ago, I mean, it's a rare disease, so there weren’t-- the area is evolving, the research is evolving. You know, the science is changing day to day.”
CHERYL PETRUK:
“Absolutely.”
JASMINE SAHNI:
“So I imagine when he was diagnosed, there weren't many resources.”
CHERYL PETRUK:
“There was nothing.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“Absolutely. So in 2014, we actually came together with a group of other patients and caregivers in Canada, and we founded the Canadian MPN Network Patient Advocacy organization because I felt well, and when he first was diagnosed, I would search for people that had the disease because it was like, we felt so alone when we left the doctor's office.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“So I'd find somebody and I would, you know, connect with them and go, “Oh my God, I found somebody else," or "Oh my gosh…" you know, so we really felt it was important to have a community. So we got together with some other folks in Canada.”
JASMINE SAHNI:
“Yeah.”
CHERYL PETRUK:
“Established the network. And today we've got support groups in every city across Canada.”
JASMINE SAHNI:
“So it initially just started off with you trying to find information for yourself.”
CHERYL PETRUK:
“Absolutely.”
JASMINE SAHNI:
“Some people going through similar situations, people to lean on, learn from their experiences, and then it morphed into a foundation that you co-founded.”
CHERYL PETRUK:
“Absolutely. Actually, I founded the, the, Canadian MPN Research Foundation. So as Eugene progressed over, you know, the, his myelofibrosis journey, I said to him, you know, we really need to do more. We need to, and he and I always we did a lot for our community. We did a lot for, you know, the organizations that we worked with, with our children, with our sons, and, and, you know, so that was kind of part of who we were.”
JASMINE SAHNI:
“And you took, what's, what was a very challenging situation that most people probably can't even imagine and turned it into something that can benefit others going through the same present day. So with all of that said, when you have a newly diagnosed patient or a family or a caregiver reach out to you, what, what would you share with them today that you wish you knew, you know, at the beginning of your journey?”
CHERYL PETRUK:
“Well, the first thing I'd say to you, Jasmine, is take a big deep breath, you're gonna be okay. Really, you're going to be fine. Yes, you might have diagnosis with a rare blood cancer, but we've got so many new evolving opportunities for patients and resources for patients. So much more now than we had 10 years ago, or 15 years ago, or 20 years ago when we were first diagnosed. And I say we, because yes, care partners, spouses, families are part of that patient, and we are diagnosed with that disease.”
“And so I would say to you, Jasmine, you're going to be okay. We've got great physicians, we've got great resources, we've got great stakeholders who are invested in helping patients live a better life. Secondly, I'd say, make sure you get a MPN specialist. Get a second opinion. So many patients are diagnosed at the HCP or primary care physician level. And unfortunately, these doctors they don't see this disease very often because it is a rare disease. So, they may put them on watch and wait, or they may discount it and say, oh, it could be this, or it could be that.”
“And, you know, get as much education about the journey that you're on and that you're about to take, whether that's patient support groups, whether that's community support you know, having a physician that you understand and like, and really, will take what they have to say and utilize it to live your best life. Because it’s important that the physicians have a longitudinal basis of their quality of life.”
JASMINE SAHNI:
“Yes. It’s pretty impressive that you just as a family went through this, didn’t really know what was happening, didn’t really have much information available to you, many resources. Now you’ve created not only an organization that benefits patients, now you’ve created an app that could even, you know, evolve the science further. It’s amazing what you’re doing and all the information you’re sharing, sharing your husband’s experience, your experience and what you’re doing with it now. I mean, I, I don’t think anyone can probably thank you enough for it.”
JASMINE SAHNI:
“Well, thank you again, Cheryl. I really appreciated our conversation and it's really these types of conversations that will help us ultimately get ahead together.”
TEXT ON SCREEN:
Mapping Myelofibrosis Logo
Explore MappingMF.com for more information.
Trademarks are owned by or licensed to the GSK group of companies.
©2023 GSK or licensor.
MMLCOCO230001 May 2023
Produced in USA.

Your Myelofibrosis Guide
Download and print the Myelofibrosis Guide so that you have important information about myelofibrosis at your fingertips.
What is myelofibrosis?
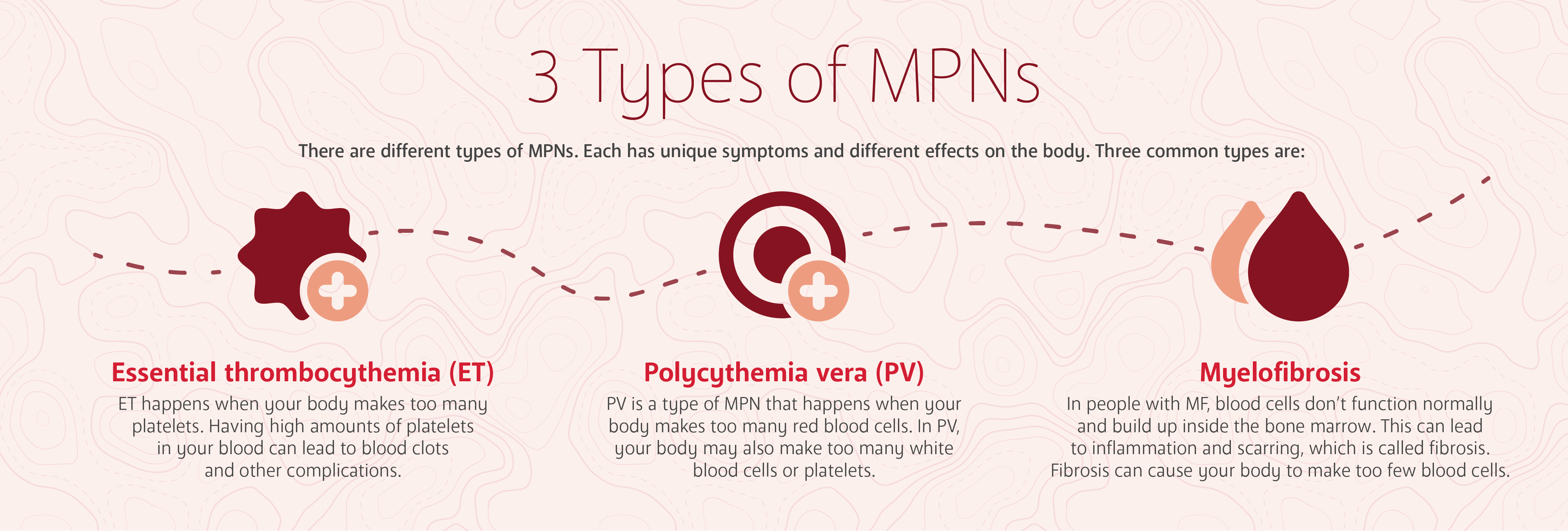
Myelofibrosis is a rare blood cancer. In the U.S., approximately 25,000 people are affected by myelofibrosis. Myelofibrosis is part of a bigger group of blood cancers called myeloproliferative neoplasms, or MPNs. MPNs affect the blood and bone marrow, which is the spongy tissue inside your bones.
Mapping Myelofibrosis with Dr. John Mascarenhas
Myelofibrosis is a chronic condition, which means that it will require management over time. By working with your healthcare team, you may be able to better navigate your symptoms. Listen as Dr. John Mascarenhas, a hematologist oncologist, explains what myelofibrosis is, how it presents and how it is diagnosed.
Transcript
TEXT ON SCREEN:
Mapping Myelofibrosis Logo
Understanding Myelofibrosis with Dr. John Mascarenhas
What is Myelofibrosis?
DR. JOHN MASCARENHAS:
Myelofibrosis is a blood cancer.
TEXT ON SCREEN:
Dr. John Mascarenhas
Hematologist Oncologist
DR. JOHN MASCARENHAS:
“So myelofibrosis is a blood cancer. It comes from the bone marrow. It results in fibrosis or scarring in the bone marrow, and often low blood counts that can really impact patients, so patients often do not feel well. They are going to have a lot of different symptoms, and it can really be debilitating. Unfortunately, it's a chronic disease, meaning it doesn't spontaneously remit. It is eventually progressive. It can progress in different ways for different patients. I'm not sure there's a typical presentation, actually. The presentations can be wide and varied. I really think it's very heterogeneous and variable the way patients present in their clinical course.”
TEXT ON SCREEN:
What are the signs and symptoms of myelofibrosis?
DR. JOHN MASCARENHAS:
“So sometimes you see patients present to a primary physician with complaints that might be protean, systemic symptoms like fevers, night sweats, weight loss. Then the workup ensues, and perhaps blood counts are abnormal. That then triggers a referral to a hematologist who then ultimately does a bone marrow biopsy and the diagnosis is made.”
“Sometimes patients end up in the emergency room, sometimes for clotting reasons, bleeding reasons, or acute issues, and then the diagnosis may be ultimately made. Then sometimes patients really are misdiagnosed or not correctly diagnosed and given a different diagnosis, perhaps like myelodysplastic syndromes or other diseases that can masquerade or be mimics of myelofibrosis, and I've seen that happen until it finally is confirmed.”
“So it really can be quite different. I don't really think any two patients really present in the exact same way and have the same course, and patients come through the door through various mechanisms, either through referrals from primary physicians, diagnosis sometimes within the hospital. Increasingly patient referrals, patients are advocates for themselves and their families are often advocates for themselves, and they will find centers of excellence because the reality is myelofibrosis and myeloproliferative neoplasms are rare diseases.”
TEXT ON SCREEN:
How is myelofibrosis diagnosed?
DR. JOHN MASCARENHAS:
“Myelofibrosis itself has to be diagnosed with a bone marrow biopsy, nowadays with mutational testing, chromosomal testing, and putting all of that together so that you meet certain World Health Organization criteria for either primary myelofibrosis or secondary myelofibrosis from an antecedent essential thrombocythemia or polycythemia vera.”
“So, getting the diagnosis is crucial because the treatments are tailored to the diagnosis and the subtypes of disease. Then I think making sure that your disease or the treatment plan for your disease is personalized and tailored to the goals of therapy for you because it really is, as I keep saying, it's variable. It's variable in how patients present their clinical course, and their treatment goals could be different.”
TEXT ON SCREEN:
Mapping Myelofibrosis Logo
Explore MappingMF.com for more information.
Trademarks are owned by or licensed to the GSK group of companies.
©2023 GSK or licensor.
MMLCOCO230009 May 2023
Produced in USA.
Exploring the signs & symptoms
Each person experiences MF differently with varying symptoms. In the early stages, approximately 1/3 of people impacted by myelofibrosis do not have any symptoms of the disease.
Additionally, the list below is not comprehensive of all the symptoms people may experience. It is important to keep track of any new or worsening symptoms, and share those with your healthcare professional, as they may be a sign of initial disease or disease progression.
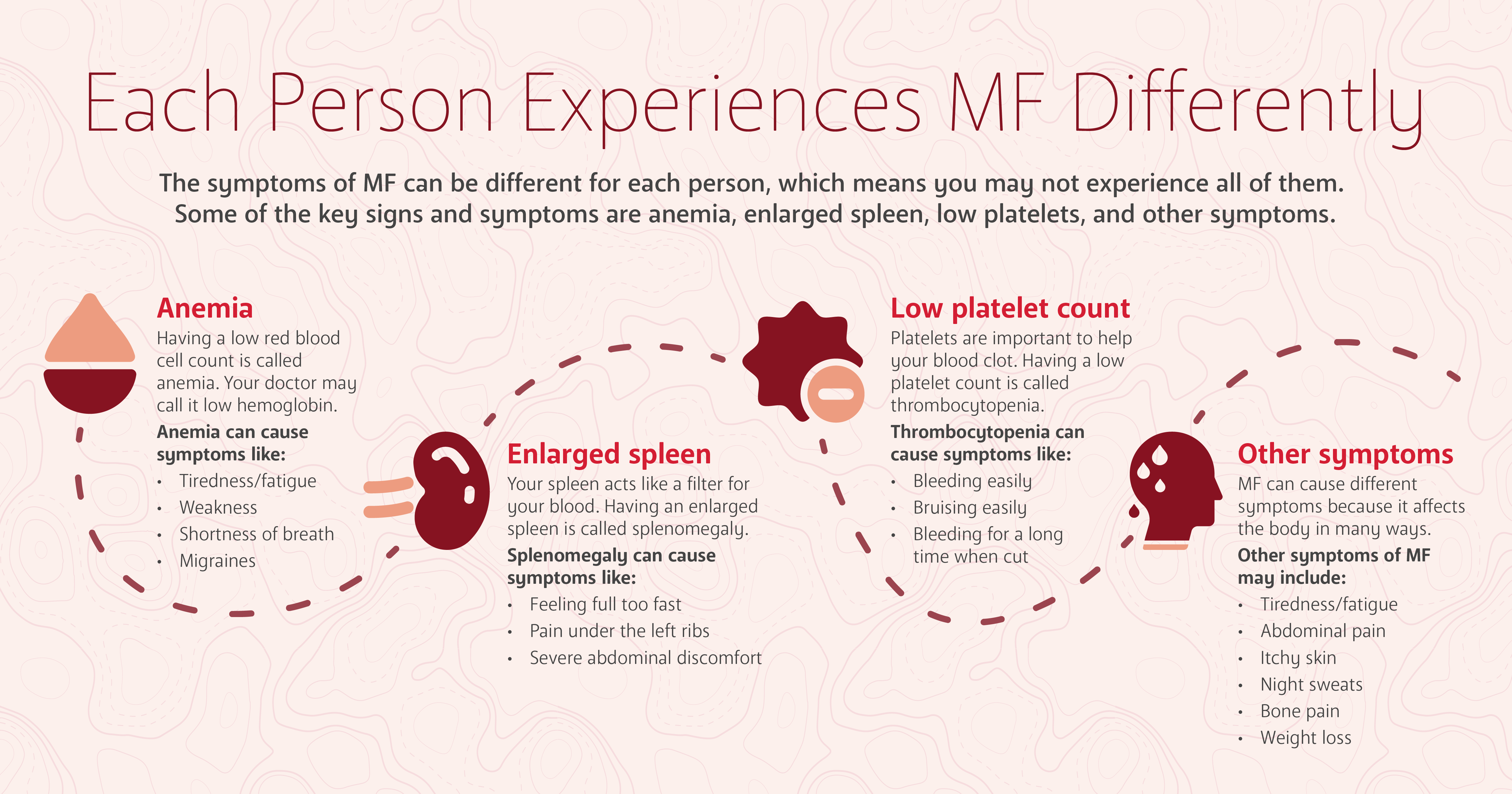
No matter what symptoms you may experience, they can have a significant impact on your daily life. Tracking and understanding your symptoms is one way to chart your course with the disease and explore disease management with your healthcare team.
Arriving at a diagnosis
Healthcare providers use the following tests and procedures to diagnose myelofibrosis:
Physical Exam
A physical exam may include a check of your vital signs, such as pulse and blood pressure, along with checks of the lymph nodes, spleen and abdomen.
Blood Tests to Check for Low Blood Cell and Platelet Counts
One test looks at your complete blood count, which may show red blood cell levels below the normal range, indicating potential anemia. White blood cell and platelet counts are also looked at and may be higher or lower than normal in some people.
Imaging Tests
Imaging tests such as X-rays, ultrasounds and MRIs may help your doctor determine more information about your MF. Your doctor will review your scans to look for the following, which may lead to a diagnosis of MF: lymphadenopathy (lymph node enlargement), osteosclerosis (generalized increased bone density), hepatomegaly (enlargement of the liver) and/or splenomegaly (enlargement of the spleen).
Bone Marrow Biopsy and Aspiration
A sample of bone tissue and marrow from your hipbone is taken out using a needle. Another type of needle may also be used during the procedure to take a sample of the liquid portion of your bone marrow. The samples are studied in a laboratory to determine the numbers and types of cells found.
Biomarker Testing
Biomarker testing is used to find biomarkers, or medical signs such as genes and proteins, that may provide information about cancer. Biomarker testing is an additional tool that can be used by healthcare providers to determine treatment options that may be right for certain patients. It can be done on a bone marrow sample to help to rule out chronic myelogenous leukemia, myelodysplastic syndrome or other chronic myeloid disorders. It can also be done via a blood draw ordered by your healthcare provider.

Living with Myelofibrosis
Whether you’ve been living with MF or are newly diagnosed, this guide can provide strategies for understanding your disease and offer tips for telling others.

MF Nutritional Considerations Resource & Recipes
This cookbook offers healthy eating options to people with or managing myelofibrosis.

What to Eat Info Sheet
Information sheet for those impacted by myelofibrosis, which includes foods to consider and limit.
*MPN Research Foundation is an independent body bringing together the voices of the patient and their caregivers living with a MPN and the researchers and clinicians seeking answers for MPN patients. MPNRF supports multiple efforts to increase awareness of MPNs and advancements of all validated, promising, and impactful approaches to better outcomes for patients.
Trademarks are property of their respective owners.
This website is funded and developed by GSK.
This site is intended for US residents only.
2023 GSK or licensor. MMLCOCO230017 August 2023
Produced in USA.