Autoimmune diseases pose challenges for patients and physicians due to their chronic, incurable nature – and lupus is no exception. Affecting at least 5 million people globally, lupus stands as one of the most difficult autoimmune diseases to diagnose and treat.[1]
May is Lupus Awareness Month, which serves as an important reminder that educating patients and physicians about this condition may have a significant impact on helping more people manage their disease earlier and more effectively. GSK’s own Liz Michel, U.S. Medical Lead - COVID Therapeutics, knows firsthand what it is like living with lupus. “Despite the breadth of knowledge we’ve gathered over the years, there is still a lot of work to be done to increase visibility and greater understanding of this disease.” Lupus patients and their caregivers may feel misunderstood or isolated because the world around them may be unfamiliar with the signs and symptoms of lupus, which is why spreading awareness about this potentially life-altering disease is critical.
Lupus may look and feel different for each patient
Lupus is an unpredictable disease and each patient experiences it differently. While its symptoms may vary from person to person, some of the most common symptoms include painful or swollen joints, extreme fatigue, unexplained fever, skin rashes and organ damage.[3]
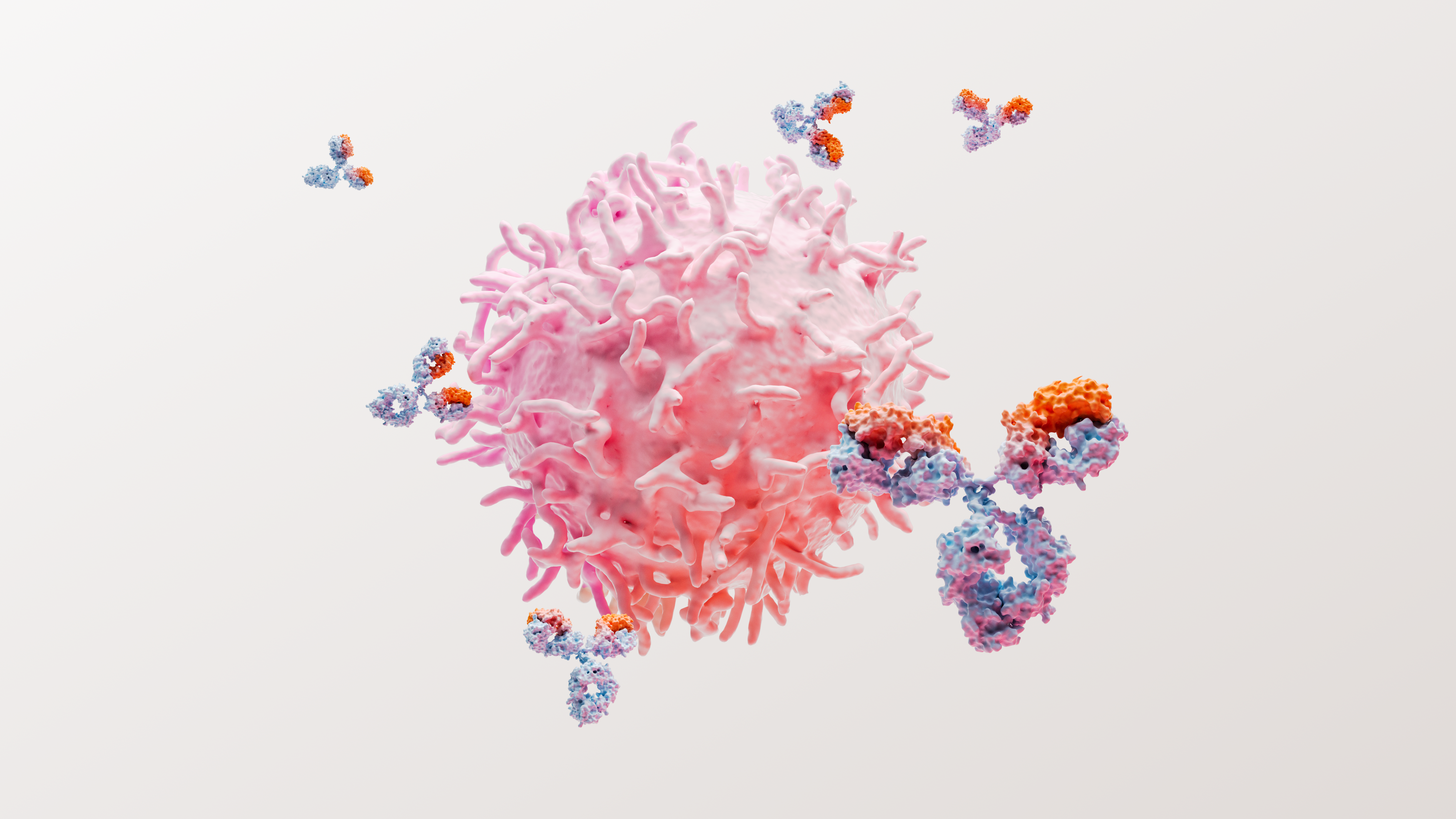
In cases of systemic lupus erythematosus (SLE), the most common form of lupus, the body produces antibodies that attack its own healthy cells and tissues in addition to producing antibodies to protect against infection.[2][3] The consequences of SLE can be profound, as persistent disease activity is associated with a higher risk of organ damage and mortality.[4]
The unpredictable and relentless nature of lupus can affect patients physically and mentally, making it one of the most challenging diseases to manage daily, both for patients and their loved ones.
Liz initially suspected something was wrong when she felt unwell while presenting at a meeting in Denver, Colorado. While she attributed the incident to altitude sickness at first, she noticed that her unusual symptoms of dizziness and nausea persisted for months afterward.
“I spent years working on the lupus team at GSK, and even with my deep knowledge of the disease, I still didn’t recognize my signs and symptoms could be lupus. After four months of doctor visits with cardiologists, endocrinologists, neurologists and eventually a rheumatologist, undergoing a spinal tap and other intense medical procedures, I finally received my diagnosis. It was a tough few months, but I was diagnosed much faster than the majority of those living with lupus, which takes on average six years.”
Understanding the long-term burden of lupus
Though lupus can be difficult to diagnose, early detection is essential to providing patients with treatment that may improve outcomes over the long-term. The unfortunate reality is that oftentimes treatment is started too late.
It is estimated that irreversible organ damage will occur in up to 50% of SLE patients within five years of diagnosis and is associated with a poor long-term prognosis and early mortality.[5],[6],[7] Additionally, approximately 40% of SLE patients globally develop lupus nephritis (LN), which is inflammation of the kidneys caused by SLE.[8] LN can lead to end-stage kidney disease, which requires kidney dialysis or a transplant and can be costly. Despite improvements in both diagnosis and treatment over the last few decades, LN remains an indicator of poor prognosis.[9],[10]
Today, Liz keeps her lupus in check by visiting her rheumatologist regularly, following the treatment regimen prescribed to her, exercising, eating well and making time for herself and her family.
Liz noted, “Most people would never guess that I have lupus. Like many patients, I don’t present with a rash and typically accommodate my activities to keep my disease in check – but that doesn’t mean we aren’t sick. Lupus can be a life-altering and debilitating disease even though it isn’t always visible. After being diagnosed, the significant unmet need for increased disease awareness and education among patients and physicians was clear to me. It’s also important to humanize the lupus journey and help patients understand how to advocate for themselves – which includes knowing what to do if you suspect you may have lupus and ensuring you have a support network around you.”
Paving a brighter future for patients
At GSK, we’re inspired by the stories of lupus patients like Liz who continue to persevere despite the burden of this relentless disease. Recognizing that proactive, early treatment is the best way to improve outcomes and prevent long-term organ damage, education around new therapy options and strong communication between not only patients and physicians, but also full care teams is paramount.
We are committed to following the science in lupus to develop a greater understanding of the disease and how treatment can be designed to help patients manage their unique needs. Building on decades of clinical evidence demonstrating success in the lupus space, we at GSK continue to seek innovative ways to bring effective treatment to those who need it most.
“I am incredibly proud of the work GSK has done to advance lupus treatment, which is fueled by a continued commitment to putting patients first. My personal experience with lupus has driven me to approach all of my work through the lens of a patient – a mantra that motivates me to help others take control of their disease and Do More, Feel Better, and Live Longer,” said Liz.
References
[1] Lupus Foundation of America. Lupus facts and statistics. Available at: https://www.lupus.org/resources/lupus-facts-and-statistics. Last accessed December 2019.
[2] Lupus Foundation of America. What is lupus? Available at: https:// resources.lupus.org/entry/what-is-lupus Last accessed March 2019.
[3] NIH National Institute of Arthritis and Musculoskeletal Diseases. Handout on health: systemic lupus erythematosus. Available at: http://www.niams.nih.gov/Health_Info/Lupus/. Last accessed: March 2019.
[4] Lopez R, Davidson JE, Beeby MD, Egger PJ, Isenberg DA. Lupus disease activity and the risk of subsequent organ damage and mortality in a large lupus cohort. Rheumatology. 2012 Mar;51(3):491-8.
[5] Chambers SA et al. Rheumatology. 2009; 48(6):673–5.
[6] Urowitz MB et al. Arthritis Care Res (Hoboken). 2012; 64(1):132–7.
[7] Segura BT et al. Rheumatology. 2020; 59(3):524–33.
[8] Hanly JG et al. Rheumatology (Oxford). 2016; 55(2): 252–62.
[9] Gordon C, Hayne D, Pusey C, et al. European Consensus Statement on the Terminology used in the Management of Lupus Glomerulonephritis. Lupus 2009;18:257-26.
[10] Waldman M and Appel GB. Update of the Treatment of Lupus Nephritis. Kidney International 2006;70:1403-1412.
[11] Waldman M and Appel GB. Update of the Treatment of Lupus Nephritis. Kidney International. 2006;70:1403-12.